80 year old with sharp, intermittent, burning pain worsened on sitting down relieved by simple steroid caudal block when all other measures failed.
41st Annual Regional Anesthesiology and Acute Pain Medicine Meeting
Thursday, March 31, 2016–Saturday, April 2, 2016 Abstract:1491
Low dose caudal epidural steroid injection for chronic pelvic pain
Preetika Kataria, Aman Upadhyay, Vivek Loomba
https://www.asra.com/content/documents/_all_presented_absracts_ra16.pdf
- 80 yr old woman
- 5 years rectal pain 8/10
- neuropathic – sharp, intermittent, burning pain
- some features pudental neuropathy – worsen problem sitting down and prolonged latency on pudental nerve EMG on right
- pudendal nerve block and subsequent ganglion impar block – no benefit
- Various neuropathic helping meds no help but we now know they only help in 23.7% cases – NSAIDs, acetaminophen and gabapentin 3600 mg daily
- caudal epidural steroid injection with 3 ml of 0.25% bupivacaine,
depomedrol 80 mg and 6 ml of 0.9% normal saline - pain dropped to 0/10 and was so at 3 week followup
Comment – I wonder it there was a sacral tarlov cyst irritating a nerve root and that is just waiting to be shut down.
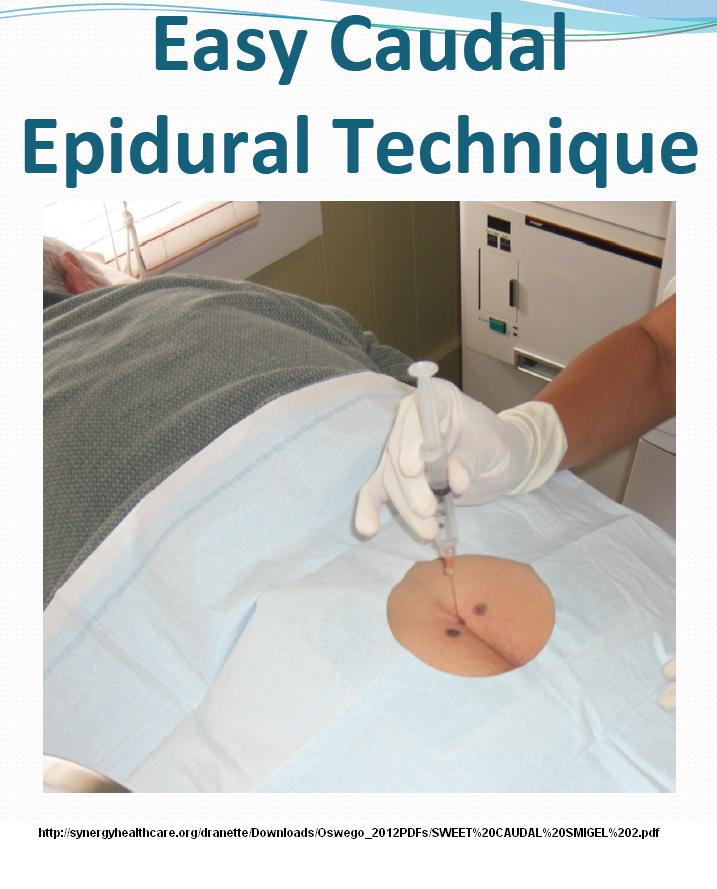
Injecting the sacral haitus can be a risky business in elderly where any advancement of needle up can be painful. The recent finding of a vertical placement of needle into hiatus with injection would help.
Anesth Pain Med. 2016 May 10;6(3):e35340. eCollection 2016.
Vertical Small-Needle Caudal Epidural Injection Technique.
Maniquis Smigel L1, Dean Reeves K2, Jeffrey Rosen H3, Patrick Rabago D4.
https://www.ncbi.nlm.nih.gov/pubmed/27826539
- use a 25 gauge 3.7 cm hypodermic needle
- if placement is not right it will be hard inject but a simple adjustment on the hole will make it work better and then patient will feel the pressure in back higher up as it goes in
that requires some depth to the sacral hiatus.
Surg Radiol Anat. 2017 in press
doi: 10.1007/s00276-017-1823-1.
Anatomy of the sacral hiatus and its clinical relevance in caudal epidural block.
Bagheri Het et al
https://www.ncbi.nlm.nih.gov/pubmed/28247084
“Depth of hiatus less than 3 mm may be one of the causes for the failure of needle insertion.” Fortunately, that occurs only 8.7% of time but I bet is more in elderly
I have a lady with complex mixture of piriformis, inferior gluteal nerve irritation, pudental neuropathy, thoracolumbar back pain, cluneal nerve pains, rib-iliac crest impingement, and gluteus medius medius bands. Much has settled down with multiple treatments but lasting benefits are elusive. I wonder if a caudal would help. Did try a sweet caudal the old fashioned way but that was painful – maybe she would go for a vertical steroid one.

I am very interested in receiving a response from you base on the following case cited above. My husband has suffered with rectal pain for about 5 years, as well. The pain usually follows a bowel movement and can last all day at the same levels cited below. Similar history of treatments, as below. Most recently he had a Caudal Epidural Steroid Injection, about 3 weeks ago. While it seemed that for 2 or 3 days (not sequential) he didn’t have the pain, the pain is now back to where it was. I wondered if a repeat Caudal Epidural Steroid Injection could potentially help and if so how soon would he be able to take it. If not, can you recommend other treatment options? The pain, as you know, is horrific and life altering.
I look forward to hearing from you as soon as possible
The case cited by you:
-80 yr old woman
-5 years rectal pain 8/10
-neuropathic – sharp, intermittent, burning pain
-some features pudental neuropathy – worsen problem sitting down and prolonged
latency on pudental nerve EMG on right
– pudendal nerve block and subsequent ganglion impar block – no benefit
-Various neuropathic helping meds no help but we now know they only help in 23.7%
cases – NSAIDs, acetaminophen and gabapentin 3600 mg daily
– caudal epidural steroid injection with 3 ml of 0.25% bupivacaine,depomedrol 80 mg
and 6 ml of 0.9% normal saline
-pain dropped to 0/10 and was so at 3 week followup
Michele:
It has been suggested that people have 3 epidurals before failure is ascribed as placement might not be adequate (there is a epidural septum that can lessen effects). I would definitely repeat epidural but only with 40 mg depo steroid.
Epidurals without steroid do have effect on back pain and can be given as often as necessary. They are given from then tailbone insertion area.
Sweet Epidural Caudal Sugar-Water Injections Cut Back Pain Longterm
http://painmuse.org/?p=5195
so might be worth trying sometime too.
If epidurals do help, then MRI imaging might need to be done to rule out sacral tarlov cysts though they are more related to coccyx/tailbone pains and sciatica:
Journal of Neurosurgery: Spine July 2001 / Vol. 95 / No. 1 / Pages 25-32
Tarlov cysts: a study of 10 cases with review of the literature
Jean-Marc Voyadzis et al
http://thejns.org/doi/abs/10.3171/spi.2001.95.1.002
I can’t help but think if blocks give momentary benefits then an inferior hypogastric block might help and can be given rather simply now:
Choi HS, Kim YH, Han JW, Moon DE.
A new technique for inferior hypogastric plexus block: a coccygeal transverse approach-A case report.
The Korean journal of pain. 2012 Jan 1;25(1):38-42.
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3259136/pdf/kjpain-25-38.pdf
However, if one thing could be done, I think a sacral stimulator might be the best answer:
Korean J Pain. 2010 Mar; 23(1): 60–64.
doi: 10.3344/kjp.2010.23.1.60
Sacral Nerve Stimulation for Treatment of Chronic Intractable Anorectal Pain -A Case Report-
Kyung Seung Yang et al
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2884202/
I would botox any local tenderness pains (though when used for treating anal fissures, too much can cause some anal leakage)
If anyone has other ideas – please share
-admin
I got a STEROID shot in the neck my right arm got hot I got up and walk ed and sat back down and yelled for help . Felt like lighting running through my back arms and legs. Shard pain in back. begged for catherator has they gave me morphine and my bladder shut down. Lightening started running through my body and kept getting stronger can walk a little now. Taking Norco 5 325 for pain helps but wears off and and tingling and numbness gets intense colon in flames get constipated and bladder in flames 2 months and I could have nerve damage. Non of the doctors want or can help me. Act like I’m going to sue and I just may. It has ruined my life and family.