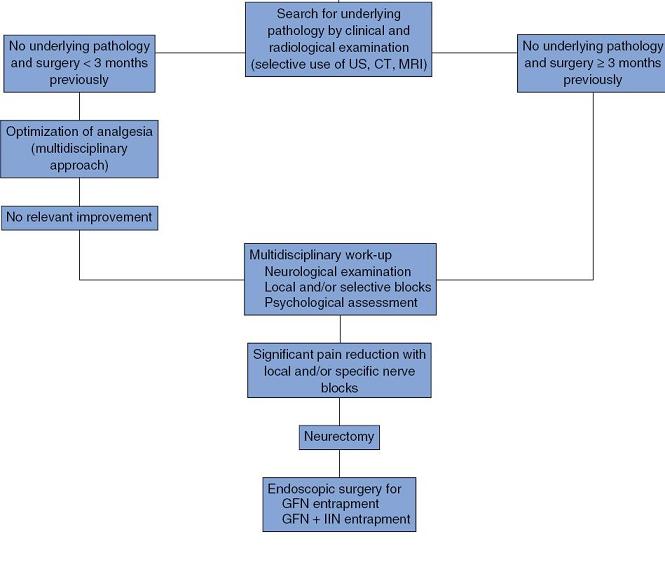
Recent Article gives a flow chart for dealing with post hernia pains – all leading to a surgical nerve removal procedure called Endoscopic retroperitoneal neurectomy.
British Journal of Surgery 2009; 96: 1076–1081
Endoscopic retroperitoneal neurectomy for chronic pain after
groin surgery
U. Giger1,2, M.N.Wente3, M. W. Buchler3, S. Krahenbu¨ hl4, J. Lerut2 and L. Krahenbuhl
This involved surgery to remove nerves.
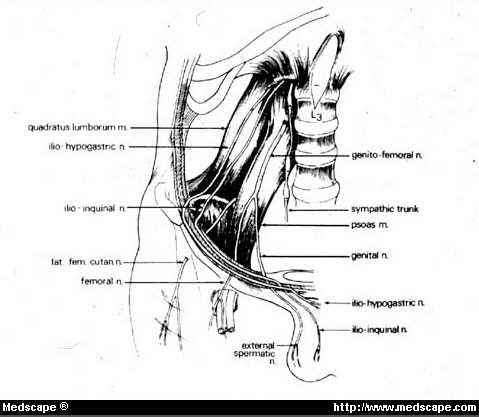
“a 4–5-cm resection of the GFN, including the bifurcation, was performed in all cases, usually at the level of the psoas muscle. When simultaneous IIN/IHN neurectomy was required, these nerves were exposed and resected proximally and laterally to the GFN where they cross the quadratus lumborum muscle.”
“RESULTS: At both timepoints after ERN, the severity of chronic postoperative groin pain at rest and during daily activities, and the rate of occupational disability, were significantly decreased in 27 of the 39 patients compared with preoperative values (all P < 0.001).”
Flow chart for managing cases is as follows (sorry pics tend to look bad for some reason):
Making a right diagnosis is critical step:
World J Surg. 2007 Sep;31(9):1760-5; discussion 1766-7.
Classifying post-herniorrhaphy pain syndromes following elective inguinal hernia repair.
Loos MJ, Roumen RM, Scheltinga MR. abstract
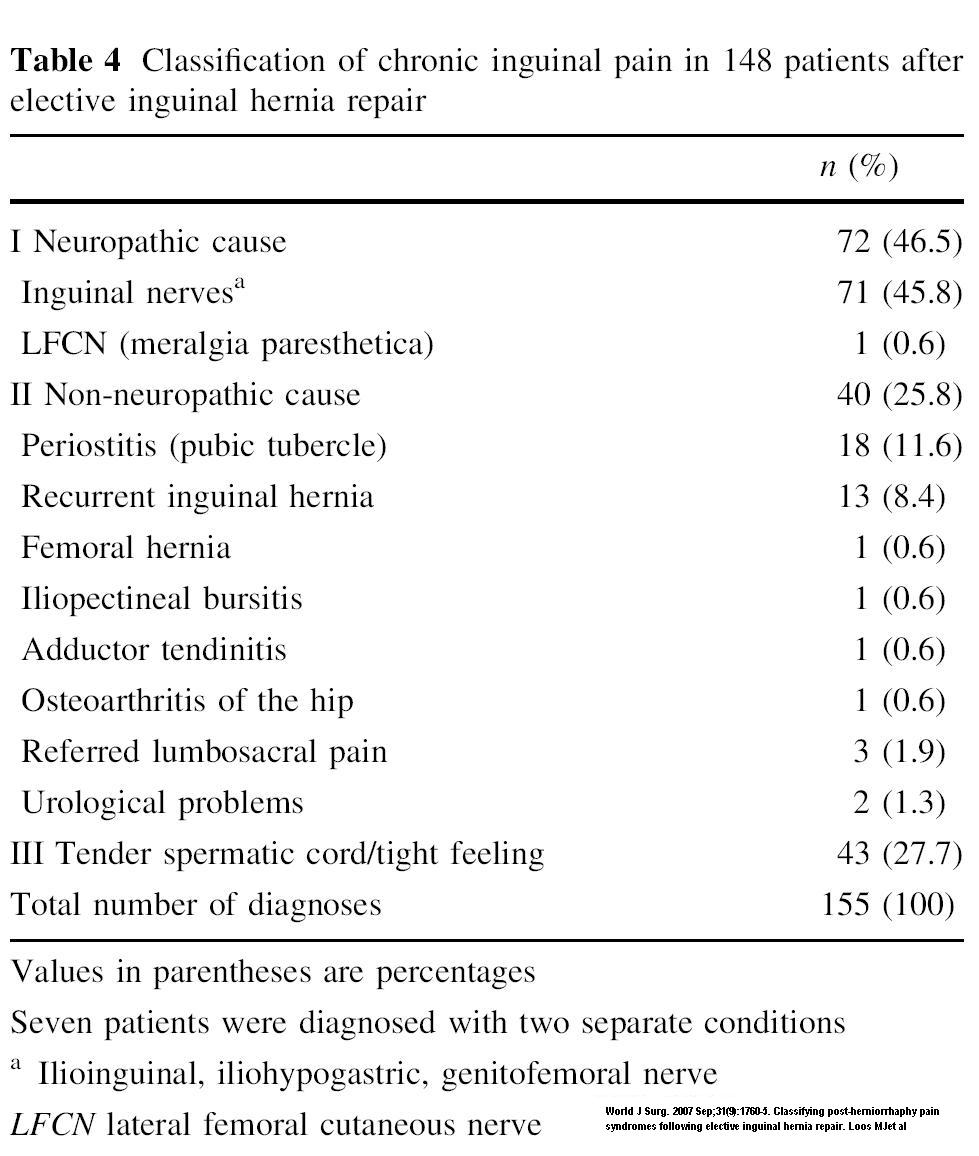
Post inguinal hernia surgery, there are a variety of causes of pain:
The periostitis of pubis tubercle
was an interesting group. The pubic tubercle is placed here (B):
They found:
“In 18 patients a periostitis pubis was diagnosed. On examination their pain was clearly situated on
the pubic tubercle, possibly as a result of an incorrectly positioned deep suture. Eight patients with a suspected periostitis received an injection with lidocaine and corticosteroids in tissue overlying the painful periosteum for diagnostic purposes. All eight participants reported pain reduction of more than 50% on their VAS-score.”
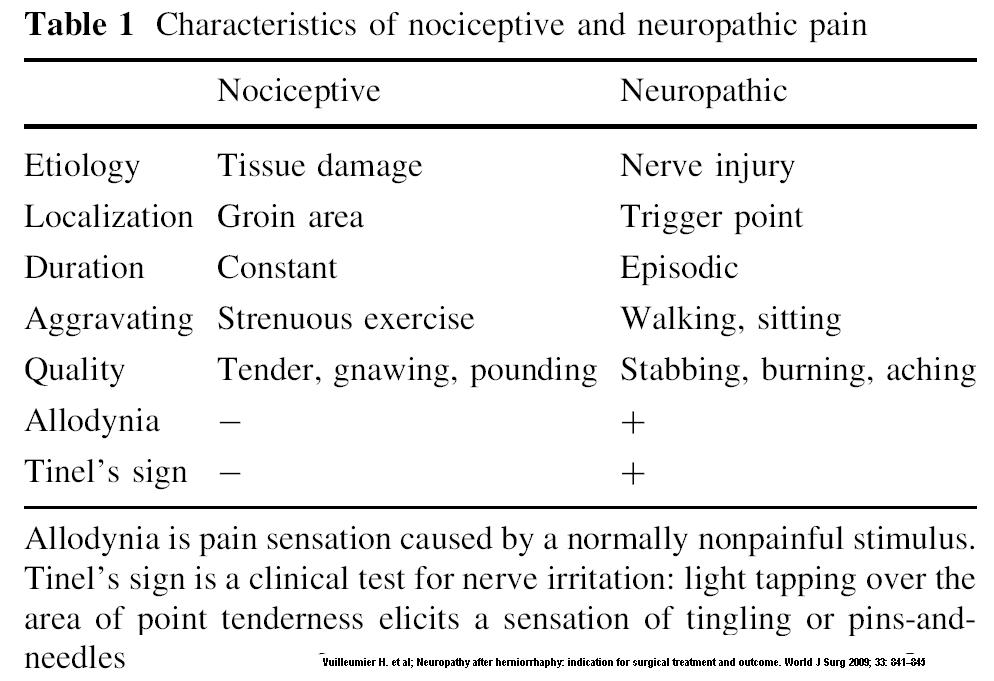
One of the first things one has to decide is if the pain is neuropathic (nerve damage) or not (nociceptive)
As you can see, the protocol weighs heavily on use of selective nerve blocks. The two nerves that tend to get most injured are the ilioinguinal and the genitofemoral nerves.
To explain how complex this can be, I had a case of testicular pain. he wanted to see and expert so I referred him to a urologist who told him he had “orchialgia”, get used to it, and avoid painkillers. The patient seemed moved by this fancy name almost to the point of it being a religious experience until I told him it meant sore testicles… He was sore just medial to the anterior superior iliac spine so did a ilioinguinal block there, This relieved the soreness locally but did not relieve the pain. He was tender near the midline abdominally so repeated block on the genitofemoral nerve. This heped some but he was still some sore. Finally, with his abdominal pain gone, I was able to tell that his pubic joint anteriorly was tender. This can be a contributor to orchialgia so I injected this joint with 40 mg Kenalog. I did not see for quite some time after as he was travelling, but when I did see, he stated he was fine, as if anyone would have expected that outcome..
Depending on the study,ilioinguinal (IIN) injuries were observed in 80 per cent and iliohypogastric (IHN) nerves in 20 per cent.:
Vuilleumier H, Hubner M, Demartines N.
Neuropathy after herniorrhaphy: indication for surgical treatment and outcome.
World J Surg 2009; 33: 841–845
and
Br J Surg. 2010 Mar 4;97(4):618. [Epub ahead of print]
Endoscopic retroperitoneal neurectomy for chronic pain after groin surgery (Br J
Surg 2009; 96: 1076-1081).
Vuilleumier H, Hübner M, Demartines N.
Top article found more Genitofemoral nerves.
Use of Neurolytic Blocks:
I would specifically look for tenderness and a tinel’s sign (shotting down numbness when tapped). I would inject area with 5% lidocaine and dextrose (plus or minus 40 mg triamcinolone) and repeat weekly until tender areas are gone. There are agents more neurolytic – absolute alcohol has been successfully used,
and Cryotherapy (freezing area) is helpful as well:
Surg Endosc. 2003 Feb;17(2):196-200. Epub 2002 Dec 4.
Cryoanalgesic ablation for the treatment of chronic postherniorrhaphy neuropathic
pain.
Fanelli RD, DiSiena MR, Lui FY, Gersin KS. abstract here
“After cryotherapy, patients reported overall pain reduction of 0% to 100% (mean, 77.5%; median, 100%); 80% reported decreased analgesic use, and 90% reported increased physical capacity. Two patients underwent additional cryotherapy, one for incomplete relief and one for recurrent pain, both with 100% efficacy. Wound infection (n = 1) was the only complication.”
Peripheral Nerve Stimulation
Another option that has been successful is peripheral nerve stimulation. There are several case studies of its use:
- Stinson LW, Roderer GT, Cross NE, Davis BE.Peripheral Subcutaneous Electrostimulation for Control of Intractible Post-operative Inguinal Pain: A Case Report Series.
Neuromodulation 2001;4(3):99-104. abstract
“Results. All three patients responded very favorably (75–100% pain relief at three, 10, and 12 months postimplantation). There were no complications. All three tapered off their pain-related medication, dramatically increased their levels of activity, and discontinued pain-related medical visits. Both patients who were on disability due to inguinal pain have been able to return to full-time employment.”
- Pain Physician. 2006;9:261-266,
Peripheral Nerve Field Stimulation in Chronic Abdominal Pain - Richard M. Paicius, MD, Clifford A. Bernstein, MD, and Cheryl Lempert-Cohen, MD
They used one electrode.
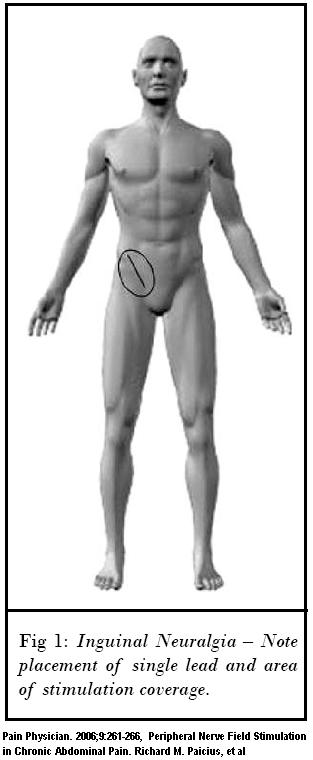
“a 14 g Tuohy needle was introduced at the superior aspect of the previous right inguinal surgical scar and advanced subcutaneously. An 8 contact electrode (Advanced Neuromodulation
Systems (ANS) Plano, Texas, Octrode 3186) was then introduced through the needle and the needle was withdrawn. The patient reported comfortable stimulation in the region of the inguinal
pain. The lead was secured, and complex programming was done using the Multiprogram Trial Stimulator (MTS trial system, ANS). The patient reported significant relief of pain during the
trial period, with average pain reported as 4/10, and the decision was made to proceed with a permanent implant.” After revision of implant, she was able to get complete relief and stop all pain meds.
- Neuralgia of the genitofemoral nerve after hernioplasty. Therapy by peripheral nerve stimulation
Der Chirurg 80(8) August, 2009, 741-744 - J. Walter1 , R. Reichart1, C. Vonderlind2, S.A. Kuhn1 und R. Kalff1 abstract here
Nearly 70% relief
There is a US site for finding a physician doing neuromodulation. It is:
http://www.sjm.com/neuromodulation/
Any experience with these procedures?

I have periostitis from a 2nd hernia operation that was performed by laperoscopic prosedure at a right inguinal hernia sight. The problem is where the screw is attatching the mesh to the pubic bone, and causing an irriation and inflammation of the membrane of the pubic bone. This pain has been going on since February of 2011 and is getting much worse.My pain level now is at a 8-9. In the past year, I’ve had at least 10 doctors and surgeons give me the runaround. I am putting myself homeless, so that I can come up with the transportation money for this surgery.