Technique involves injecting ilioinguinal nerve (by anterior superior iliac spine) – with dye and local – if get GOOD temporarly relief – then go in right after and remove all dye stained areas including ilioinguinal nerve.
In selected cases (good relief with block) 27/28 cases had pain for relief for at least the year of study.
Am J Surg. 2013 Jan 25. [Epub ahead of print]
Directed neurectomy for treatment of chronic postsurgical neuropathic pain.
Kline CM, Lucas CE, Ledgerwood AM. abstract here
Technique:
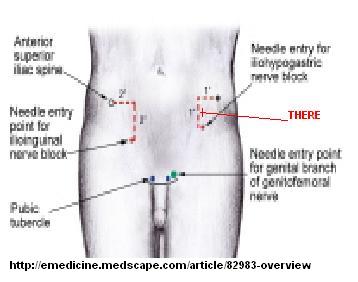
1) inject local just medial and little down from anterior superior iliac spine: (“often 2 cm medial and 2 to 3 cm inferior to the respective anterior superior iliac spine”)
- To make mixture use 1 mL of vital blue dye(methylene blue) added to 3 to 5 mL .5% bupivacaine.
- Try to use only 1 ml of mixture (might need a nerve probe or get good referral zinger – I would just use my pointer plus at 1.5).
- Sedate patient ?midazolam 0.5 – 1 ml and ?ketamine 15-30 mg im deltoid
- Only procede if get good block of pain – wait and see
- 2-3 cm incision
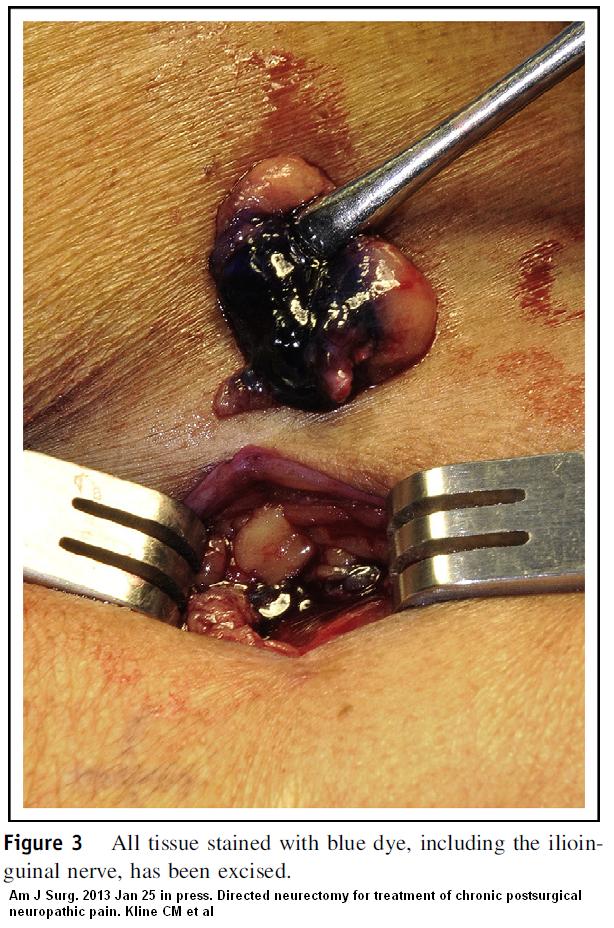
- Remove the subcutaeous plug of tissue down to external oblique fascial layer where dye is
- “The stained tissue that contained the nerve was found posterior to the external oblique fascia. All of this more posterior blue-stained tissue, which was below the subdermal fat, was excised (Fig. 3). The blue-stained tissue, which was removed typically, contained a small amount of deep subcutaneous fat and a portion of the external oblique fascia; there may have been a small
portion of the internal oblique muscle. The involved nerve was usually observed in the resected tissue. “ - “The wound was closed with absorbable interrupted sutures”
Comment – all hernia surgeons should have to learn this technique if they think they intend to do hernia surgery – they should have to fix their complications. From image obtained above, it may be more complex then one incision – above had two to get to extent of dye. Having said that, it does not look difficult at all.
For a methylene blue source, all I could easily find was Vista-Blue™ – Methylene Blue Solution – sterile vials used more in dentistry available at:
http://vista-dental.com/products/query.cfm?id2=Methylene
Could use more sources…
The authors come from Department of Surgery, Wayne State University, 4201 St Antoine, Suite 4V, Detroit, MI 48201, USA. The corresponding author is Dr. Charles E. Lucas, M.D., Tel.: 11-313-745-3485; fax: 11-313-993-7729.
E-mail address: clucas@med.wayne.edu
Sorry about this Charles, but I think untreated desperate cases might need to contact him for advice – though if they failed to get any temporary relief from blocks elsewhere there would be no point …. Many anesthetists would try an ilioinguinal alcohol block there first though I think surgery would be more definitive.

Hi, Had a laprascopic hernia repair rhs done in 2005,then had my left side done in 2011. This was done in an open incision and mesh placed over sight. Never been fully pain free. Right side causes pain on ejaculation,and left side had some discharge from scar sight for a couple of years. Then 9mths ago I removed a stitch from the sight. I believed the stitches were meant to be dissolving.
Then in 2012 I had a back injury,believed to be L4/L5 facet joint. Physio,ultrasound,electro stimulation therapy,helped to restore my back enough to return to work. Had a reoccurrence in 2013 and another in 2014. This is still unresolved. The so called experts are not sure now if it’s facet joint or sacro iliac joint. Have tried all the past treatments including iontopherisis,steroid injection to sacro iliac joint and a nerve block to L4/L5 facet joint,all to no avail.
Now part of my treatment involved doing clinical pilates. The varies exercises,core strengthening etc,put strain on my already weak stomach muscles and caused severe pain,predominantly left side,whilst working,walking,twisting or even just sitting.
ultrasound showed some abnormality,but unclear as to whether it was a reoccurrence or just clumping of the mesh. His answer was to just take analgesics for pain and put up with it. Not happy with that,so got a second opinion. He believes pain is from sutchers either in my pelvic bone or my pubic tuberal. He has injected cortisone to site and now awaiting outcome.
Interested in any points of view,and is it possible,after some of the research I have done,that the back and hernia pain could be related?
If so,any ideas on next course of plan,or in particular,is this back pain something I must live with?
Thank you.
———-
You’re right – the back will be involved.
Pain tends to regionalize- all structures in area can become involved. If you pinch the skin you might find it tender all the way to the back where ribs end. I find the skin nerve (ilioinguinal, iliohypogastric, genitofemoral) will become tender all the way to the level of the back where ribs end and that level will be in spasm and the facet back joints sore as well. As well as injecting tender site where things started, then I inject each cm. with a skin bleb of sugar water D5W going all the way to back. If back paraspinous muscles are spastic I inject the with 5% lidocaine laterally and work out. I also use an activator device to manipulate those levels. Any residual soreness in thoracolumbar junction I relieve by positional release – lie on stomach and raise thigh on affected side up with a pillow until thoracolumbar facet areas not tender and then hold in that position for 90 seconds. This needs multiple repetitions.
Good luck.
admin