Opioids for chronic pain: Taking stock – editorial
Pain – in press Sept 2006
Discusses a study finding people on opioids were not better off. I feel they failed to comprehend that poor copers may be the ones that need opioids most and were not better off to start with.
They do mention studies showing that opioids do improve quality of life:
Portenoy and Foley, 1986 – increased pain control, better quality of life and low addiction rates
Kalso et al., 2004 – increased pain control, increased function but study limited to 8 weeks.
They however refer to a Danish study:
Eriksen J, Sjogren P, Bruera E, Ekholm O, Rasmussen NK. Critical issues on opioids in chronic non-cancer pain. An epidemiological study.
Pain 2006; doi:10.1016/j.pain.2006.06.009.
This study found:
” found that opioid users reported significantly more moderate/severe or very severe pain, poorer self-rated health, and lower quality of life scores than opioid non-users. They also identified significant associations between opioid use and low levels of physical activity and employment, and high levels of healthcare utilization. Even after controlling for pain intensity”
Comment – there is a big difference between pain and disability. A mindset has to be present for the latter. This mindset could actually be genetically driven – I had one genetist tell me there was work being done on a “catastrophizing gene”. There appears to be some genetic link to PTSD as well. Those who are more disabled may need more opioids. -And of course they appear to be functioning less well.
Most “functioning” evaluations primarily consider back to work as the indication of improvement. In Denmark, with its excellent health plan, you may not see this back to work. I remember some years ago Danish studies were unable to demonstrate any back to work improvement on tertiary programs. They complained that American studies were able to get patients back to work only because they didn’t give them enough to live on elsewise.
There does seem to be a misunderstanding on the potency of opioids. Generally there will only be a 20-50% reduction in pain level. Occasionally, a patient wants more and will take themselves up to disabling levels of opioids in the process.
Dr. Dennis Turk, one of the fathers of the biopsychosocial model for treating chronic pain by cognitive-behavioural techniques etc. points to his research finding “Opioids reduce severe, chronic pain by only about a third. Moreover, up to 50% of patients discontinue opioid therapy because of a lack of efficacy or because of side effects.”
http://painmuse.org/ref/turk.pdf
This only highlights the need for use of accessory medications like tricyclic antidepressants and anti-convulsants.
An issue with the above has been my expereince that “I have never met a patient with Fibromyalgia(FM) that didn’t have a bad stomach for pills”. The high rates of Irritable bowel in FM translate into high rates of esophagitis because it is a total gut dysmotility problem. I have given up trying to treat these subjects with medications without first putting them on a PPI (Proton pump inhibitor). The may also need Dicetel but of course our drug plan has seen fit to not cover it. They also need to realize that their facilitated transmission of pain means facilitated transmission of side effect “noise” as well and the first week on any medication they are not going to feel so hot.
When I began using opioids, I thought I would no longer be required to do trigger injections and the like. This was my biggest disappointment. Their decreased pain would be translated into increased activity and hence restoration of their prior pain levels. Pacing education became important. – But they all want to take that killer holiday (where there is a “ledge” with their name on it for them to trip on…)
Addendum:
Recent damning study:
A longitudinal study of the efficacy of a comprehensive pain rehabilitation program with opioid withdrawal: Comparison of treatment outcomes based on opioid use status at admission
Cynthia O. Townsend *, Jennifer L. Kerkvliet, Barbara K. Bruce, Jeffrey D. Rome, W. Michael Hooten, Connie A. Luedtke, John E. Hodgson
Use of opioids for chronic non-cancer pain is controversial and the efficacy of comprehensive pain rehabilitation programs (CPRPs) that incorporate opioid withdrawal requires further investigation. We test the hypothesis that patients with chronic pain and longstanding opioid use who undergo opioid withdrawal in the course of rehabilitative treatment will experience significant and sustained improvement in pain and functioning similar to patients who were not taking opioids. A longitudinal design study compared 373 consecutive patients admitted to the Mayo Clinic Pain Rehabilitation Center at admission, discharge and six-month post treatment by opioid status at admission. Measures of pain severity, depression, psychosocial functioning, health status, and pain catastrophizing were used to assess between- and within-group differences. Treatment involved a 3-week interdisciplinary pain rehabilitation program focused on functional restoration. Over one-half of patients (57.1%) were taking opioids daily at admission. The majority of patients (91%) completed rehabilitation and 70% of patients who completed the program returned questionnaires six months posttreatment. On admission, patients taking low- and high-dose opioids reported significantly greater pain severity (P = .001) and depression (P = .001) than the non-opioid group. Significant improvement was found on all outcome variables following treatment (P < .001) and six-month posttreatment (P < .001) regardless of opioid status at admission. There were no differences between the opioid and non-opioid groups upon discharge from the program or at six months following treatment.
Conclusion: Patients with longstanding CPRP on chronic opioid therapy, who choose to participate in interdisciplinary rehabilitation that incorporates opioid withdrawal, can experience significant and sustained improvement in pain severity and functioning
——-
Unfortuantely what it means is biased:
Selection bias:
1) Best copers – Only those coping well enough to agree to “detoxification”
2) Only cases coping well enough to afford such a program.
3) Mentally stable – “Discontinuation of these medications is not recommended for patients, who use these drugs to treat comorbid medical or psychiatric illnesses.” – so must have pre-selected these people out.
4) High academic cases – average grade level 14.6
5) Cases in which opioids unlikely to be of much use:
a) Generalized Musculoskeletal and low back pain = 8.8% + 24.4% = 33.2%
According to a study on opioid use these catagories without arthritis had the poorest response rate to opioids:
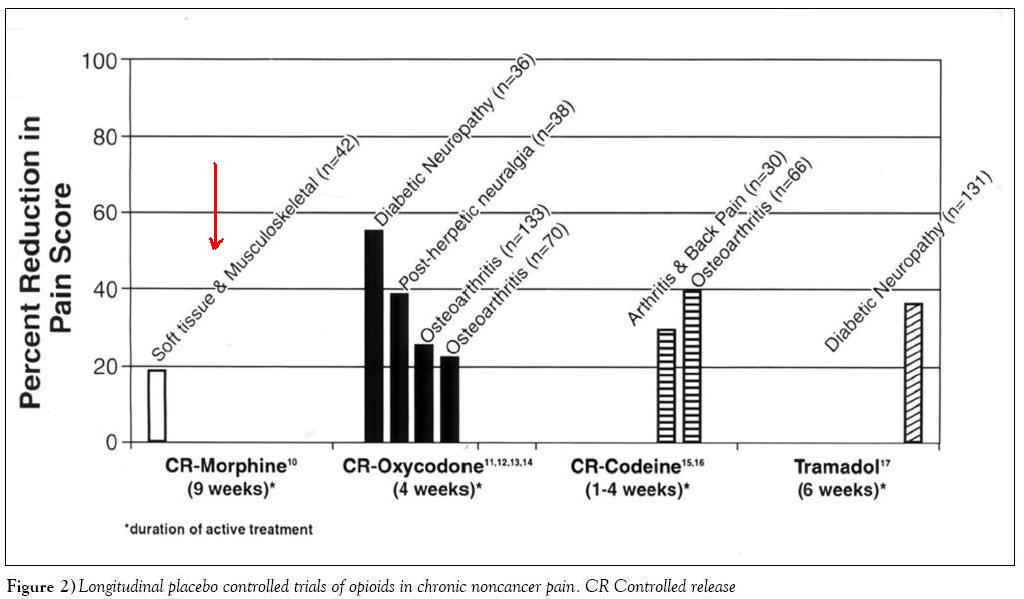
(from: Pain Research & Management
Winter 2002, Volume 7 Issue 4: 179-184
Chronic pain in Canada – Prevalence, treatment, impact and the role of opioid analgesia
DE Moulin, AJ Clark, M Speechley, PK Morley-Forster
b) Fibromyalgia 19.8% – many authors state opioids ineffective there
c) Chronic headaches and migraines 11.5% – of course opioids make them worse with rebound headaches and analgesic induced chronic daily headaches
d) Abdominal pains 7.2%– consider situation – you have a constipating condition, you take opioids which makes you super-constipated, you then have to take laxatives which cause painful bowel spasms – no winning there…
e) Neck pains – 6.4% – if aggravated by headaches then c) applies again
f) Unspecified – 21.9% – anyone’s game here
6) Been on opioids so long not likely to be much use anymore (mean 3.9 years)
7) No mention of WCB: “Over one quarter (106; 28.4%) of the patients in this study population were working for wages at the time of admission to the rehabilitation program. Less than one-fifth (62; 16.6%) of the patients were involved in on-going litigation related to their chronic pain. Over
one quarter (100; 26.8%) of the patients were receiving disability assistance (short- and long-term), and almost one-tenth of the study cohort (41; 11.0%) were in the process of applying for disability.”
8) Program allows them to get well enough without opioids – “Pain rehabilitation in this setting incorporates physical therapy, occupational therapy, biofeedback and relaxation training, stress management, wellness instruction (e.g., sleep hygiene, healthy diet), chemical health education and pain management training (e.g., activity moderation, elimination of pain
behaviors).” – most programs do not have the physiotherapy and occupational therapy so this treatment option might not work.
9) Leave out the tough ones – No mention of neuropathic, no spinal cord injuries, no CRPS –just the easier ones likely to respond to treatment so that opioids may no longer be necessary.
Authors should be congratulated concerning stacking the deck so they could get the results they wanted and still making it look academic.
Having said that, they make the same sort of complaint about opioid literature:
“ However, evidence of long-term improvements in pain and functioning attributable to opioid therapy is lacking. Meta-analyses and reviews of randomized, double blind, placebo-controlled trials of opioids for CNCP [chronic non-cancer pain] found these trials were of brief duration (average 5 weeks), subject to publication bias from pharmaceutical company sponsorship, and limited by significant dropout rates and eligibility criteria that excluded subjects with depression and a history of substance abuse
[6,14,23,27,29,35]. The trials did not demonstrate that opioids provide a sustained reduction in pain severity or improvements in function and mood.”
Nevertheless, the accusation of “there is evidence that opioid-induced hyperalgesia and opioid tolerance can exacerbate pain and subvert the clinical utility of opioid therapy” is disturbing…
Annoyingly, “detoxification” alone without a rehab program appears not to have been done – leaving way too many confounding factors. Did have one case “detoxified” off opioids and left to subsist in a fetal position while her parents looked after her son – only to be restarted on opioids some ? months later.
addendum:
Functional Outcomes in Patients with Chronic Nonmalignant Pain on Long-Term Opioid Therapy
Authors: Soin, Amol; Cheng, Jianguo; Brown, Lora; Moufawad, Sami; Mekhail, Nagy
Pain Practice, Volume 8, Number 5, September/October 2008 , pp. 379-384(6)
- Cohort of 67 patient prior to and 6-36 months after starting opioids
- Improved physical functioning, physical role, bodily pain, general health, validity, social functioning, emotional role, and mental health.
- No significant changes were observed in reported health transition, VAS pain scores, disability status, or return to work
It is clear that at least initially, opioids offer the most effective treatment for chronic pain. With no chance to access to a pain clinic with multi-disciplines including physio and occupational therapy, options become more limited. I believe much of the pain is peripherally based and working these areas will make a difference (2/10 down anyway).
I would be interested in other peoples perspective re this…
I would be interested in other comments on this issue and any ways of managing the frustrations…

Opioids don’t seem to be the answer at all for some. Turk rated lack of efficacy in 50%. A Canadian study put it at over 1/3.
CMAJ. 2006 May 23; 174(11): 1589–1594.
Opioids for chronic noncancer pain: a meta-analysis of effectiveness and side effects
Andrea D. Furlan, Juan A. Sandoval, Angela Mailis-Gagnon, and Eldon Tunks
http://www.cmaj.ca/cgi/content/full/174/11/1589