I have become aware of two cases of chronic pain following a Stretococcal infection. This could be a flavour of an Ankylosing Spondylitis with sacroiliits being a prime factor. As a matter of fact in those patients with persistently elevated Antistretolysin titers (ASO titers) suggestive of chronic strep infection, “Most of the subjects with high ASO titer had unclassified or undifferentiated arthritis.”
as per:
Evidence-based correlation between anti-streptolysin O serum titer and sacroiliac joint disorder
Chang ST (Chang, Shin-Tsu), Ku CH (Ku, Chih-Hung), Cherng SC (Cherng, Shiou-Chi)
JOURNAL OF RHEUMATOLOGY 34(8): 1746-1752; AUG 2007 abstract
Conditions:
Acute Post- Streptococcus Reactive Arthritis:
1) Post – Streptococcus infection – strep throat, streptococcus septicemia, strep skin infection.
2) In adults, peak age is 21- 37 for onset.
3) Initially in adults, 46% had multiple joint involvement, 35% a few joints, and 19% had one joint affected. 81% of time condition was “non-migratory” – ie not jumping from joint to joint. Acutely, joints often affected included knee, ankle, hip, and wrist.
4) 66% had frank reactive arthritis lasting over 6 weeks, while arthralgias could persist after that.
5) While spinal arthritis was seen in only 2% of cases, if subject was HLA-B27 positive (known to be related to Ankylosing spondylitis as well), then incidence was 24%
6) Flare condition with recurrent infections and persistent Penicillin use can help prevent these flares.
Chronic Post Streptococcus Reactive Arthritis
1) Persistent sensitization indication – persistently elevated ASO titers with “Most of the subjects with high ASO titer had unclassified or undifferentiated arthritis”
2) Arthrtis responds poorly to NSAID’s “arthritis with poor responsiveness to salicylates/non-steroidals”
Rheumatology 2005 44(1):136
Poststreptococcal reactive arthritis (PSRA): a plea for diagnostic criteria
T. L. T. A. Jansen, M. Efde and A. Spoorenberg free article
3) Spinal involvement especially SI joints (as per #1 above). Pain is deep, dull, maximal over SI joint areas – ie parasagittal sacrum
4) If radiation, to thigh only
5) Patrick’s test was always positive!
6) Signs of inflammation – ESR, CRP – most often normal
7) Poor response to NSAID’s
8) Rare cases of soft tissue inflammation noted – supraspinatus or achilles tendonitis, dorsum foot tenosynovitis, adductor enthesitis (sore groin to knee area), dactylitis (sore swollen fingers)
9) Rare rashes – leukocytoclastic or necrotizing vasculitis rash – non blanching red spots, perhaps a bit lumpy, rarely forming ulcers.
10) MRI or SI joint scintigraphy might be positive in a research setting but I have not been convinced radiologists have had enough experience (and the equipment is advanced enough) to make a diagnosis here.
11) In all cases that were HLA-B27 positive (a marker used in kidney etc transplants) – all had spondylitis after early episode of post strep reactive arthritis
12) Fatigue is common in Ankylosing spondylitis so expect would be here too : Turan Y, Duruöz MT, Bal S, Guvenc A, Cerrahoglu L, Gurgan A.Assessment of fatigue in patients with ankylosing spondylitis.Rheumatol Int. 2007 Jul;27(9):847-52. Epub 2007 Jan 25.PMID: 17252263
TNF inhibitors like Etanercept (Enbrel) are now licenced for use in ankylosing spondylitis(AK) and found useful in AK with mixed connective tissue disease:
Yonsei Med J. 2008 Feb 29;49(1):159-62. Successful etanercept therapy for refractory sacroiliitis in a patient with ankylosing spondylitis and mixed connective tissue disease. Lee JY, Chang HK, Kim SK.
With Post Streptococcal reactive arthritis, it would seem prudent to keep on Penicillin while taking Enbrel.
Comment: This has a low potential for being diagnosed because:
1) Can’t see it – spinal
2) Poor response to arthritis pills – even I would have trouble diagnosing without a response to therapy
3) Normal ESR and CRP – blood work is no help
4) Xrays are normal and more involved imaging requires machinery and expertice I am not convinced is available here.
5) Women with the disorder will be confused with sacroiliac disease, a condition aggravated by the ligamentous loosening in pregnancy.
6) In women, I see this being confused with Fibromyalgia. I would only diagnose FM after treatment with Enbrel failed.
7) The major finding, though obviously not very specific, was a Positive patrick’s test:
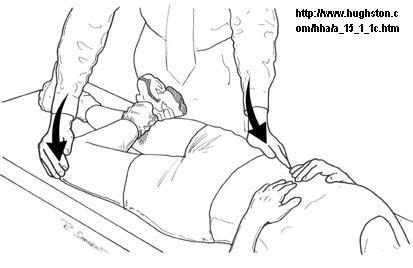
Push knee down and brace opposite anterior pelvic brim – Look for pain IN THE BACK.
8) That finding, along with a positive blood test for ASO titer would be highly suspicious.
9) A short course of Prednisone (with a statin to help prevent osteonecrosis), or a Kenalog 60 mg IM shot (with statin coverage) could potentially unmask the inflammatory nature.
Anyone had experience with or have this condition?

My daughter got severe arthritis in her wrists following a strep infection. She has had low grade fevers and rashes. The arthritis did not respond to NSAIDs and Mri shows some edema and erosion. Her pediatric rheumatologist is convinced its systemic juvenile arthritis, but other respected rheumatologists thinks it’s post strep reactive arthritis. Her ASO titer is well over 1000 and she had protein and red blood cells in her urine. My doctor does not want her to go on a prophylatic penicillin but all other doctors think she should. She will be starting a short course of prednisone and methotrexate. What i have concluded is that this is an art, not a science, and that the doctors really don’t know for sure.
I have had strep throat for 2 weeks now, the first perscription drug i took wasnt strong enough, so i got put on stronger ones… over the last 4 days i have had pains in my wrists, thumbs, fingers, elbows, knees, ankles, toes shoulder….. everyday a different joint hurts more then others.. coming and going, i have had 2 bloodtests and discovered i do have PSRA……… doctor tells me to take my prescriptions for the infection of my strep, and high dose of aspirin 4 times daily.. not working out yet.. where do i go from here, i need to go back to work one day…
My nephew has been in the UCSF hospital for 34 days and counting. He was initially diagnosed with a Behcet’s like syndrome with Necrotizing Vasculitis. Today, test results show that he has the HLA B27 gene and now they are thinking it is Reactive Arthritis. However, the Drs said they are confused because he has vasculitis instead of colitis. I think I just figured it out. He has had several bouts with strep throat and he may have Post-Streptococcus Reactive Arthritis with Necrotizing Vasculitis.
Poor guy. He is 22 and used to weigh 165 lbs. He now weighs 95 pounds. Send some positive thoughts to California.
My son haas been diagnosed with reactive arthritis. He is presently in Southern California. Does anyone know a specialist there he could see? They say they are 90% sure that is what he has. He is 23 years old. Why the weight loss for Debra Snell’s Nephew?
I had septicemia and toxic shock when my last child was born, despite asking my doctor for antibiotics, I wasnt given penicillin till 10 days after. This led to toxic shock and reactive arthritis in my si joint. It was undiagnosed for 3 months despite being EXTREMELY painful and aggravated when in ICU and the ward. A bone scan finally showed the INTENSE inflammation 4 months after it occurred.
i will be very happy having imformation about the different type of asthritis and their cause. especially aso asthritis. i am a victim of the disease. and the cue for the disease. it the disease inheritate?thanks
I have been sick since Nov of 2010 with various sinus infections, bronchitis, etc but never once diagnosed with strep. As soon as I would complete a round of anti-biotics I would be sick again with fever, sore throat, aches and pains. It was the joint pain that was so incredibly painful; after suffering with worsening joint pain for 3 months Ifinally went to my PCP and blood work immediately showed signs of PSRA. I have never heard of such a disease!! I have been out on disability for 3 weeks now and the pain continues to move from joint to joint. I am on prednisone and penicillin and just miserable. I am unable to take any form of anti inflammatory medications due to severe stomach problems. Is there any hope for a full recovery? I cannot stand to be on prednisone anymore. Miserable…
Justtrying to see if others feel as sore and frustrated with interest of medical profession as i am at present.positive asot and history of reccurent sore throat over the winter.Sudden onset of sore fingers,wrists,knees,ankles and toes since late january.no improvement with naproxen,paracetamol and recent commencement of low dose amitryptiline. A five minute private consultation ended with one shot of IM steroid and the comment that if it doesnt help i have fibromyalgia which he said there was no treatment. Cant afford to stay off work but know i am too sore to stand in work! Any advice welcome
I have suffered with chronic joint pain and fatigue for years now. My ASO titer stays elevated ; last test was >800. Prednisone is helpful for the initial flare ups but terrible longterm. I find myself always seeking for a quick cure but never find one. The one thing I do recommend is: At the initial onset of a sore throat or illness, seek medical treatment. Strep screen should be performed as this will exacerbate overall symptoms if not treated appropriately.